Tools & Information | Blue Cross and Blue Shield of Alabama - Medicare
Breadcrumb
Tools & Info Banner

Tools & Resources Content
Helpful Tools
Helpful Tools
Medicare Member Documents 2025-26 release
Help Tool
Choose Documents to Show:
Member Materials (Blue Advantage):
Plan Policies (Blue Advantage):
Notices (Blue Advantage):
Member Materials (BlueRx):
Plan Policies (BlueRx):
Notices (BlueRx):
Member Materials (C Plus):
Plan Policies (C Plus):
Notices (C Plus):
Frequently Asked Questions:
-
A Medicare Advantage Plan is a Medicare approved program that allows you to have all the rights and protections of Original Medicare. Your Medicare benefits, however, will be provided by a private insurance company such as Blue Cross and Blue Shield of Alabama. This plan enhances your Original Medicare Benefits by adding Part D drug coverage and offering lower copayments. This plan does not require a supplemental plan.
-
To be eligible for Blue Advantage you must be a resident of Alabama. You must continue to pay your Medicare Part B premium (unless paid for you by Medicaid or another third party). You must also be entitled to and enrolled in Medicare Parts A & B. To be eligible for Medicare you must be 65 years of age or on disability. Our contract with CMS is renewed annually and the availability of coverage beyond the current contract year is not guaranteed.
-
If you have more than one address, you will need to provide your permanent physical address on your application. This address must match your primary address as listed with Social Security and Medicare. Your address will be used to determine your product eligibility and plan premiums. Failure to report your correct address can delay the processing of your application or result in the loss of coverage. If needed, you may also provide an alternate address (such as a Post Office Box) for billing and/or correspondence.
-
- You can view available plans and rates here.
- Premium rates for Blue Advantage plans are based on the benefit design and overall utilization of medical services.
- With all options, you are required to continue paying your Medicare Part B premium unless otherwise paid for by Medicaid or another third party. If you qualify for Extra Help, your premium may be reduced.
-
What additional benefits are offered if I elect the Blue Advantage Premier Plan at a higher premium?
- $0 primary care physician (PCP) copay
- Low copays for inpatient and outpatient hospital services
- Low copays for doctor's office visits with specialists
- $0 drug deductible
- Additional cost-savings on therapy services, radiology and diagnostic services as well as many other benefits
- $1,000 dental allowance
-
Premiums are always due on the 1st of the month and are considered late if not received by the 10th.
There are several ways you can pay your plan premium:
- Automatic monthly payment by E-Check, Credit Card, or Debit Card
- Over the telephone with Visa, MasterCard, Discover or E-Check
- Automatic deduction from your monthly Social Security or Railroad Retirement Board benefits check
- Mail a check
- Set up online bill payment through your financial institution. Please be sure to include your contract number when setting up online bill payment.
-
The Annual Election Period allows you to make changes to your plan anytime between October 15 and December 7. Elections made during this time will be effective on January 1 of the following year. When Medicare has been notified of your election change, your membership with your previous MAPD and/or Part D plan will be cancelled effective December 31. To cancel coverage other than Medicare Advantage or Part D Plans (like Medicare Supplement/Medicare Select plans), please contact your insurance carrier.
-
A current Medicare Advantage plan enrollee is allowed to make a one-time change during the Medicare Advantage Open Enrollment Period, which takes place from January 1 to March 31 or the last day of the 3rd month after their Part A and B entitlement date. This period allows you to disenroll from a Medicare Advantage plan and return to your Original Medicare- change from one Medicare Advantage plan to another Medicare Advantage plan or from one Part D plan to another Part D Plan.
Other times that you are allowed to make changes to your coverage outside of AEP are:
- Initial Coverage Election Period (ICEP) - three months before your Medicare eligibility effective date, the month of your Medicare eligibility date, and three months after.
- Special Election Period (SEP) - You can change plans anytime during the year if you gain, lose, or have a change in your dual eligible or Extra Help status. You are also allowed to make elections within 60 days of the day you lose coverage with your employer and within 60 days of the day you move into a new coverage area.
-
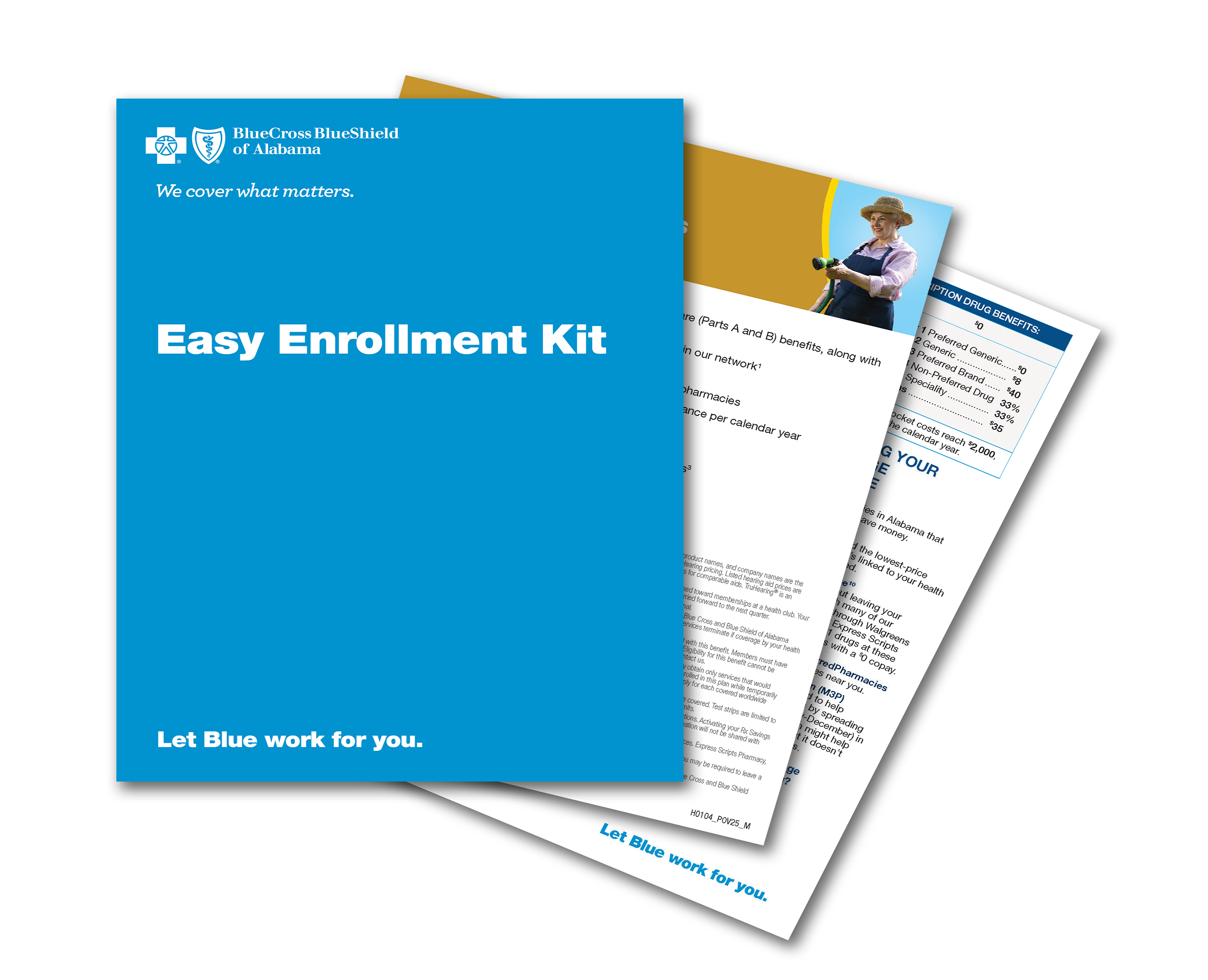
There are several ways to submit your enrollment application:
- Online
- Call us at 1-888-543-9212 (TTY 711) Monday – Friday, 8 a.m. to 8 p.m. CST. From October 1 to March 31, the hours of operation are Monday – Sunday, 8 a.m. – 8 p.m. CST. You may be required to leave a message for calls made after hours, weekends and holidays. Calls will be returned the next business day.
- Attend a local meeting
- Mail us an application or request an enrollment kit packet to be mailed to your house.
-
Your membership will end the last day of the month prior to when your new plan's coverage begins.
-
Blue Advantage offers a large network of providers who are willing to serve you.
To see if an Alabama provider participates in the Blue Advantage network, you may:
Visit our online doctor finder.
Call the Member Services number at 1-888-234-8266 (TTY 711) (non-members may call 1-888-543-9212 TTY 711) Monday – Friday, 8 a.m. to 8 p.m. CST. From October 1 to March 31, the hours of operation are Monday – Sunday, 8 a.m. – 8 p.m. CST. You may be required to leave a message for calls made after hours, weekends and holidays. Calls will be returned the next business day.
Request that a Provider Directory for your county be mailed to you.
Outside of Alabama, medical emergencies and visits to an Urgent Care Facility will process at an in-network benefit level, regardless of whether the provider is in the Blue Advantage network. For all other services outside of the coverage area, facility and provider participation may vary. To find out if an out-of-state facility or provider participates in the Blue Advantage network, contact Member Services.
-
Yes; we offer a 24-hour Nurse Line to our members. This line is available 24 hours, 7 days a week for members who have general questions concerning their health. You can reach the Nurse Line at 1-800-896-2724 (TTY 711). Although this service is available, please remember to always consult your doctor or pharmacist concerning any new services or upon taking any new medications.
-
Blue Cross has several programs in place, such as our health management and disease management programs, to help reduce the cost of health care. Blue Cross nurses actively work with members to provide support for chronic conditions, such as diabetes and heart disease, so our members can improve their overall health and wellness.
-
The Centers for Medicare & Medicaid Services (CMS) uses a five-star quality rating system to measure the experiences Medicare beneficiaries have with their health and drug plans and health care system — the Star Rating Program. Health and drug plans are rated on a scale of 1 to 5 stars, with 5 being the highest.
The Star Rating Program is intended to:
- Raise the quality of care for Medicare beneficiaries
- Strengthen beneficiary protections
- Help people compare health and drug plans more easily
View the Blue Advantage Star rating.
-
- Call us at 1-888-543-9212 (TTY 711) Monday – Friday, 8 a.m. to 8 p.m. CST. From October 1 to March 31, the hours of operation are Monday – Sunday, 8 a.m. – 8 p.m. CST. You may be required to leave a message for calls made after hours, weekends and holidays. Calls will be returned the next business day.
- Sign up to attend a meeting with a local representative. For accommodations of persons with special needs at meetings, call 1-888-246-7023 (TTY 711)
-
This plan is only available to Alabama residents. Please note that failure to report an address change can result in the loss of your coverage.
If you move within the state of Alabama, you are still eligible to keep your Blue Advantage plan; however, premium and plan options may vary based on the county that you live in. Please contact our Member Services to advise of an address change and to determine if your move will constitute any changes to your plan.
If you move outside of Alabama, Medicare will allow you 60 days from the day you move to enroll into another MAPD or Part D plan that is located in your new state. If you are temporarily moving out of the coverage area, you are allowed to have a temporary address for up to 12 months. You are responsible for notifying us if your living status changes from a temporary to permanent residence or of any permanent changes to your physical address.
-
Medicare requires all Medicare Advantage and Prescription Drug plans to notify members of the upcoming year's changes by September 30 of each calendar year.
-
ID cards do not expire and will not be issued annually. If you need a new ID card, please contact Member Services at 1-888-234-8266 (TTY 711), Monday - Friday, 8 a.m. to 8 p.m. Central Time. From October 1 to March 31, the hours of operation are Monday - Sunday, 8 a.m. to 8 p.m. Central Time. You may be required to leave a message for calls made after hours, weekends and holidays. Calls will be returned the next business day.
-
Please contact the Social Security Administration to see if you are required to reapply for Extra Help each year. There is no guarantee that you will automatically qualify each year, as the income criteria is subject to change. The Social Security Administration can be reached at 1-800-772-1213 (TTY 711). If eligible for Extra Help, Social Security will send you a letter advising of your level of eligibility. Blue Cross and Blue Shield of Alabama will also be notified of any changes to your Extra Help eligibility.
-
If your modified adjusted gross income, as reported on your IRS tax return, is above a certain amount, you will pay an extra amount in addition to your monthly plan premium. You may also hear this referred to as a surcharge, and can get more information on it here. If you have to pay an extra amount, the Social Security Administration (SSA) will send you a letter to advise what the extra amount is and how to pay it.
-
If you would like update the account you are using for automatic monthly draft or change your payment method, please call the customer service number located on the back of your ID card or log into your myBlueCross account. In the meantime, you are responsible for making sure your plan premium is paid on time.
-
To see if a specific drug is covered under Blue Advantage you may:
- View formularies online: Choice, Complete and Premier
- Look up your drug in our Drug Search tool
- Call Member Services at 1-888-234-8266 (TTY 711) (non-members call 1-888-543-9212 TTY 711) Monday – Friday, 8 a.m. to 8 p.m. CST. From October 1 to March 31, the hours of operation are Monday – Sunday, 8 a.m. – 8 p.m. CST. You may be required to leave a message for calls made after hours, weekends and holidays. Calls will be returned the next business day.
- Request that a formulary be mailed to you by calling Member Services at the number above.
-
To request coverage for a medication not on the formulary, contact your physician and ask that a formulary exception request form be submitted on your behalf. This process can take up to 72 hours for a standard request. If your life, health or ability to regain maximum function may be at risk by waiting for a standard request decision, we will let you know our decision within 24 hours. This is considered an expedited request. If a non-formulary medication is approved to be added to your formulary, the copay will process as a Tier 4.
You may also contact Member Services at 1-888-234-8266 (TTY 711), 8 a.m. to 8 p.m., seven (7) days a week. From October 1 to March 31, the hours of operation are Monday – Sunday, 8 a.m. – 8 p.m. CST. You may be required to leave a message for calls made after hours, weekends and holidays. Calls will be returned the next business day.
-
Prescription Drug Claim Form
Send your request for payment, along with receipts documenting the amount paid, to:Part D Claims
PO Box 20970
Lehigh Valley, PA 18002-0970 -
Yes, we offer the convenience of having your medications purchased through our mail order program. Click here to view more information.
-
Blue Cross and Blue Shield of Alabama offers a number of standard Drug Utilization Management (DUM) services such as formulary management, prior authorization, quantity limits and step-therapy. These programs encourage safe, appropriate and cost-effective use of drugs. The goal of DUM is to monitor and prevent over- and under-utilization of prescription drugs while respecting the physician's prescribing authority. Using DUM, we also track and trend utilization, identify opportunities for improvement, and document and implement corrective actions when necessary. All policies are reviewed quarterly by an independent committee of pharmacists and physicians.
-
The MTM Program is a free service offered by your plan that can help you keep your medications on the right track. To learn more about the MTM Program go here.
-
Prime Therapeutics LLC is an independent company that provides pharmacy solutions for Blue Cross Blue Shield of Alabama members.
-
CMS collects information about Medicare beneficiaries’ experiences with, and ratings of, Medicare Advantage (MA-only) plans, Medicare Advantage Prescription Drug (MA-PD) plans, and stand-alone Medicare Prescription Drug Plans (PDP) by participating in the Consumer Assessments of Health Plans Study (CAHPS) Survey. To review the CAHPS survey results please visit www.MA-PDPCAHPS.org
-
The Part D LIS provides extra help for people with Medicare who have limited income and resources by helping to pay their Medicare Prescription Drug Benefit costs (plan monthly premiums, co-payments, and the annual deductible). Please go to the following Social Security Administration website for more information and to see if you qualify: www.ssa.gov/medicare/prescriptionhelp
-
Medicare Prescription Drug Plans provide coverage for prescription drugs and are offered by private insurance companies approved by Medicare, like Blue Cross and Blue Shield of Alabama.
-
Medicare prescription drug coverage provides peace of mind by protecting you from unexpected drug expenses. Once you become Medicare eligible, you are required to have creditable prescription drug coverage. Failure to enroll in a Part D plan when you become Medicare eligible will result in the assessment of a Late Enrollment Penalty (LEP). This penalty will be added to your Part D premium.
-
To enroll in BlueRx, you must be a resident of Alabama or Tennessee. (If you are a Tennessee resident, please visit UTIC Insurance Company.) You must also be entitled to Medicare Part A and/or enrolled in Medicare Part B due to age or disability. You must continue to pay your Part B permium (unless it is paid for by Medicaid or another third party). Our contract with CMS is renewed annually and the availability of coverage beyond the current contract year is not guaranteed.
-
If you have more than one address, you will need to provide your permanent physical address on your application. This address must match your primary address as listed with Social Security and Medicare. Your address will be used to determine your product eligibility and plan premiums. Failure to report your correct address can delay the processing of your application or result in the loss of coverage. If needed, you may also provide an alternate address (such as a Post Office Box) for billing and/or correspondence.
-
- You can view available plans and rates here.
- If you qualify for Extra Help, your premium may be reduced based on the level of subsidy for which you qualify.
-
A current Prescription Drug Plan plan enrollee is allowed to make a one-time change during the Medicare Advantage Open Enrollment Period, which takes place from January 1 to March 31 or the last day of the 3rd month after their Part A and B entitlement date.This period allows you to disenroll from a Prescription Drug Plan plan and return to your Original Medicare, change from one Medicare Advantage plan to another Medicare Advantage plan or from one Part D plan to another Part D Plan.
Other times that you are allowed to make changes to your coverage outside of AEP are:
Initial Coverage Election Period (ICEP) - three months before your Medicare eligibility effective date, the month of your Medicare eligibility date, and three months after.Special Election Period (SEP) - You can change plans anytime during the year if you gain, lose, or have a change in your dual eligible or Extra Help status. You are also allowed to make elections within 60 days of the day you lose coverage with your employer and within 60 days of the day you move into a new coverage area.
-
There are several ways to submit your enrollment application:
- Online
- Call us at 1-888-543-9212 (TTY 711) 8 a.m. to 8 p.m., seven (7) days a week. From October 1 to March 31, the hours of operation are Monday – Sunday, 8 a.m. – 8 p.m. CST. You may be required to leave a message for calls made after hours, weekends and holidays. Calls will be returned the next business day.
- Attend a local meeting.
- Mail us an application or request an enrollment kit packet to be mailed to your house.
-
Your membership will end the last day of the month prior to when your new plan's coverage begins.
-
Premiums are always due on the 1st of the month and are considered late if not received by the 10th.
There are several ways you can pay your plan premium:
- Automatic monthly payment by E-Check, Credit Card, or Debit Card
- Over the telephone with Visa, MasterCard, Discover or E-Check
- Automatic deduction from your monthly Social Security or Railroad Retirement Board benefits check
- Mail a check
- Set up online bill payment through your financial institution. Please be sure to include your contract number when setting up online bill payment.
-
The Centers for Medicare & Medicaid Services (CMS) uses a five-star quality rating system to measure the experiences Medicare beneficiaries have with their health and drug plans and health care system — the Star Rating Program. Health and drug plans are rated on a scale of 1 to 5 stars, with 5 being the highest.
The Star Rating Program is intended to:
- Raise the quality of care for Medicare beneficiaries
- Strengthen beneficiary protections
- Help people compare health and drug plans more easily
View the BlueRx Star rating.
-
- Call us at 1-888-543-9212 (TTY 711) Monday – Friday, 8 a.m. to 8 p.m. CST. From October 1 to March 31, the hours of operation are Monday – Sunday, 8 a.m. – 8 p.m. CST. You may be required to leave a message for calls made after hours, weekends and holidays. Calls will be returned the next business day.
- Sign up to attend a meeting with a local representative. For accommodations of persons with special needs at meetings, call 1-888-246-7023 (TTY 711)
-
To see if a specific drug is covered under BlueRx, you may:
- View formularies online: Essential orEnhanced Plus
- Look up your drug in our Drug Search tool
- Call 1-800-327-3998 (TTY 711) Monday – Friday, 8 a.m. to 8 p.m. CST. From October 1 to March 31, the hours of operation are Monday – Sunday, 8 a.m. – 8 p.m. CST. You may be required to leave a message for calls made after hours, weekends and holidays. Calls will be returned the next business day.
- Request that a formulary be mailed to you
-
To request coverage for a medication not on the formulary, contact your physician and ask that a formulary exception request form be submitted on your behalf. This process can take up to 72 hours for a standard request. If your life, health or ability to regain maximum function may be at risk by waiting for a standard request decision, we will let you know our decision within 24 hours. This is considered an expedited request. If a non-formulary medication is approved to be added to your BlueRx Essential formulary, the copay will process as a Tier 4.
You may also contact Customer Service at 1-800-327-3998 (TTY 711) 8 a.m. to 8 p.m., seven (7) days a week. From October 1 to March 31, the hours of operation are Monday – Sunday, 8 a.m. – 8 p.m. CST. You may be required to leave a message for calls made after hours, weekends and holidays. Calls will be returned the next business day.
-
Yes, you are still able to purchase your medications while traveling throughout the United States. BlueRx has a nationwide network of participating pharmacies that will allow you to purchase your medicine at the same copays as you would pay at a participating pharmacy in Alabama. To find a list of participating pharmacies, please visit www.myprime.com, contact your Member Services Department, or call and request a pharmacy directory. If you use a pharmacy that is not participating, higher costs may apply.
-
Medicare requires all Medicare Advantage and Prescription Drug plans to notify members of the upcoming year's changes by September 30 of each calendar year.
-
ID cards do not expire and will not be issued annually. If you need a new ID card, please contact Member Services at 1-800-327-3998 (TTY 711), Monday - Friday, 8 a.m. to 8 p.m. Central Time. From October 1 to March 31, the hours of operation are Monday - Sunday, 8 a.m. to 8 p.m. Central Time. You may be required to leave a message for calls made after hours, weekends and holidays. Calls will be returned the next business day.
-
Please contact the Social Security Administration to see if you are required to reapply for Extra Help each year. There is no guarantee that you will automatically qualify each year, as the income criteria is subject to change. The Social Security Administration can be reached at 1-800-772-1213 (TTY 711). If eligible for Extra Help, Social Security will send you a letter advising of your level of eligibility. Blue Cross and Blue Shield of Alabama will also be notified of any changes to your Extra Help eligibility.
-
If your modified adjusted gross income, as reported on your IRS tax return, is above a certain amount, you will pay an extra amount in addition to your monthly plan premium. You may also hear this referred to as a surcharge, and can get more information on it here. If you have to pay an extra amount, the Social Security Administration (SSA) will send you a letter to advise what the extra amount is and how to pay it.
-
If you would like update the account you are using for automatic monthly draft or change your payment method, please call the customer service number located on the back of your ID card or log into your myBlueCross account. In the meantime, you are responsible for making sure your plan premium is paid on time.
-
This plan is only offered to Alabama and Tennessee Residents. Medicare will allow you 60 days from the day you move to enroll in a Part D plan in your new state.
Please contact our Member Services to notify us of any changes to your physical address. Failure to report an address change can result in the loss of your coverage.
-
Prescription Drug Claim Form
Send your request for payment, along with receipts documenting the amount paid, to:Part D Claims
PO Box 20970
Lehigh Valley, PA 18002-0970 -
Yes, we offer the convenience of having your medications purchased through our mail order program. Click here to view more information.
-
Blue Cross and Blue Shield of Alabama offers a number of standard Drug Utilization Management (DUM) services such as formulary management, prior authorization, quantity limits and step-therapy. These programs encourage safe, appropriate and cost-effective use of drugs. The goal of DUM is to monitor and prevent over- and under-utilization of prescription drugs while respecting the physician's prescribing authority. Using DUM, we also track and trend utilization, identify opportunities for improvement, and document and implement corrective actions when necessary. All policies are reviewed quarterly by an independent committee of pharmacists and physicians.
-
The MTM Program is a free service offered by your plan that can help you keep your medications on the right track. To learn more about the MTM Program go here.
-
Prime Therapeutics LLC is an independent company that provides pharmacy solutions for Blue Cross Blue Shield of Alabama members.
-
CMS collects information about Medicare beneficiaries’ experiences with, and ratings of, Medicare Advantage (MA-only) plans, Medicare Advantage Prescription Drug (MA-PD) plans, and stand-alone Medicare Prescription Drug Plans (PDP) by participating in the Consumer Assessments of Health Plans Study (CAHPS) Survey. To review the CAHPS survey results please visit www.MA-PDPCAHPS.org
-
The Part D LIS provides extra help for people with Medicare who have limited income and resources by helping to pay their Medicare Prescription Drug Benefit costs (plan monthly premiums, co-payments, and the annual deductible). Please go to the following Social Security Administration website for more information and to see if you qualify: www.ssa.gov/medicare/prescriptionhelp
-
A Medicare Supplement (Medigap) policy works with Original Medicare, picking up as a Supplement where Medicare leaves off. It covers most of the deductibles, copays and coinsurance not covered by Medicare. These policies do not cover Part D prescription drugs.
-
You can enroll in C Plus if you are an Alabama resident and enrolled in Medicare Part A and Medicare Part B. If you receive full Medicaid or Qualified Medicare Beneficiary (QMB) program benefits, you are not eligible to purchase C Plus or any other Medicare supplement. Those who are under age 65 and have Medicare due to end-stage renal disease (ESRD) may not be eligible. Coverage may be available for individuals who are disabled and under the age of 65.
-
Premiums for C Plus Plans are based on your age at the time of enrollment. The age category you start with is the one you keep as long as you're continuously enrolled in that C Plus plan. Your premium never "jumps" to the next age category.
-
C Plus is a health insurance policy only and does not provide coverage for Part D prescription drugs. You may want to enroll in one of our prescription drug plans, BlueRx (PDP), for the most comprehensive coverage.
-
Enroll in C Plus by completing the online application. You can also call one of our representatives to enroll by phone or to request an enrollment kit at 1-888-543-9212 (TTY 711), 8 a.m. to 8 pm., 7 days a week. From December 8 to September 30, on weekends and holidays, you may be required to leave a message. Calls will be returned the next business day.
An annual C Plus open enrollment will be offered each year to coincide with Medicare's Annual Election Period from October 15 to December 7. During this open enrollment, members can enroll or switch plans with an effective date of January 1. To enroll outside of the annual enrollment period, you must meet certain qualifications such as turning 65. For a complete list of enrollment guidelines, please refer to the Plan B, Plan F or Plan G contract book.
-
Premiums are always due on the 1st of the month and are considered late if not received by the 10th.
There are several ways you can pay your plan premium:
- Automatic monthly payment by E-Check, Credit Card, or Debit Card
- Over the telephone with Visa, MasterCard, Discover or E-Check
- Automatic deduction from your monthly Social Security or Railroad Retirement Board benefits check
- Mail a check
- Set up online bill payment through your financial institution. Please be sure to include your contract number when setting up online bill payment.
-
If you are covered under an employer sponsored retiree plan, please check with your employer to determine what would happen should you choose to leave your retiree plan. Sometimes, leaving makes you ineligible to return to that plan in the future. It's best to assess your current health care needs and compare how you will be covered under your retiree plan to how you would be covered under Blue Advantage (PPO), or BlueRx and C Plus prior to making a change. If your employer does not offer retiree coverage or if you believe that Blue Advantage, BlueRx or C Plus coverage may be better for you, you can enroll online, attend a meeting with your local representatives, or call 1-888-543-9212 (TTY 711), Monday – Friday, 8 a.m. to 8 p.m. CST. From October 1 to March 31, the hours of operation are Monday – Sunday, 8 a.m. – 8 p.m. CST. You may be required to leave a message for calls made after hours, weekends and holidays. Calls will be returned the next business day.
-
To attend a meeting with your local representative, call 1-888-543-9212 (TTY 711) Monday – Friday, 8 a.m. to 8 p.m. CST. From October 1 to March 31, the hours of operation are Monday – Sunday, 8 a.m. – 8 p.m. CST. You may be required to leave a message for calls made after hours, weekends and holidays. Calls will be returned the next business day. For accommodations of persons with special needs at sales meetings, call 1-888-685-6330 (TTY 711) 8 a.m. to 8 p.m., 7 days a week.
Annual Notice of Change Complete
This is important information on changes in your Blue Advantage coverage.
We previously sent you the Annual Notice of Change (ANOC) which provided information about changes to your coverage as an enrollee in our plan. This notice is to let you know there are updates to your ANOC. Within this document you will find information describing and further detailing the updates to your ANOC. These updates are due to additional information regarding the Inflation Reduction Act that was released on November 7, 2022. Please keep this information for your reference.
Evidence of Coverage Complete
This is important information on changes in your Blue Advantage coverage.
Your Evidence of Coverage (EOC) provides information about your coverage as an enrollee in our plan. This notice is to let you know there have been updates made to your EOC. Within this document, you will find information describing and further detailing updates made to your EOC. These updates are due to additional information regarding the Inflation Reduction Act that was released on November 7, 2022. Please keep this information for your reference.
Annual Notice of Change Premier
This is important information on changes in your Blue Advantage coverage.
We previously sent you the Annual Notice of Change (ANOC) which provided information about changes to your coverage as an enrollee in our plan. This notice is to let you know there are updates to your ANOC. Within this document you will find information describing and further detailing the updates to your ANOC. These updates are due to additional information regarding the Inflation Reduction Act that was released on November 7, 2022. Please keep this information for your reference.
Evidence of Coverage Premier
This is important information on changes in your Blue Advantage coverage.
Your Evidence of Coverage (EOC) provides information about your coverage as an enrollee in our plan. This notice is to let you know there have been updates made to your EOC. Within this document, you will find information describing and further detailing updates made to your EOC. These updates are due to additional information regarding the Inflation Reduction Act that was released on November 7, 2022. Please keep this information for your reference.





Third Party Website Disclaimer
You are about to leave the Blue Cross and Blue Shield of Alabama Medicare products website to visit one of our social media sites. Although content of our social media sites is maintained by Blue Cross, Blue Cross does not control the security and/or privacy practices of these external social media sites. Therefore, Blue Cross advises users of these sites against sharing any personal health information or any other information the user would otherwise not feel comfortable being made public. Blue Cross shall not be liable for privacy breaches, security incidents or similar events due to the use of social media sites.
To continue, click "Accept." If you want to stay on the Blue Cross and Blue Shield of Alabama Medicare website, click "Cancel."